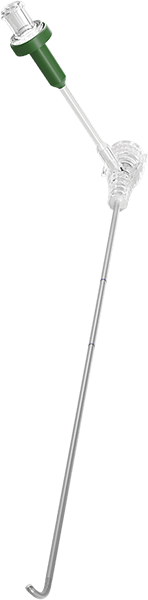
Dorsal Root Ganglion Therapy (DRG) Therapy
Prescription And Safety Information
Read this section to gather important prescription and safety information. For specific indications, contraindications, instructions, warnings, precautions, and adverse effects about system components available in your country or region, see the approved clinician's manual for those components.
Intended Use
This neurostimulation system is designed to deliver low-intensity electrical impulses to nerve structures. The system is intended to be used with leads and associated extensions that are compatible with the system.
Indications For Use
This neurostimulation system is indicated for spinal column stimulation via epidural and intraspinal lead access to the dorsal root ganglion as an aid in the management of moderate to severe chronic intractable* pain of the lower limbs in adult patients with complex regional pain syndrome (CRPS) types I and II.**
*Study subjects from the ACCURATE clinical study had failed to achieve adequate pain relief from at least two prior pharmacologic treatments from at least two different drug classes and continued their pharmacologic therapy during the clinical study.
**Please note that in 1994, a consensus group of pain medicine experts gathered by the International Association for the Study of Pain (IASP) reviewed diagnostic criteria and agreed to rename reflex sympathetic dystrophy (RSD) and causalgia as complex regional pain syndrome (CRPS) types I and II, respectively. CRPS II (causalgia) is defined as a painful condition arising from damage to a nerve. Nerve damage may result from traumatic or surgical nerve injury. Changes secondary to neuropathic pain seen in CRPS I (RSD) may be present, but are not a diagnostic requirement for CRPS II (causalgia).
Contraindications
This neurostimulation system is contraindicated for patients who are
Patients who failed to receive effective pain relief during trial stimulation are contraindicated to process to the permanent implant procedure.
MRI Safety Information
Some models of this system are Magnetic Resonance (MR) Conditional, and patients with these devices may be scanned safely with magnetic resonance imaging (MRI) when the conditions for safe scanning are met.
For more information about MR Conditional neurostimulation components and systems, including equipment settings, scanning procedures, and a complete listing of conditionally approved components, refer to the MRI procedures clinician's manual for neurostimulation systems (available online at medical.abbott/manuals).
For more information about MR Conditional products, visit the Abbott Medical product information page at http://neuromodulation.abbott/MRI-ready.
Warnings
The following warnings apply to this neurostimulation system.
Clinician training. Implanting physicians should be experienced in the diagnosis and treatment of chronic pain syndromes and have undergone surgical and device implantation training for dorsal root ganglion (DRG) neurostimulation systems.
Pregnancy and nursing. Safety and effectiveness of neurostimulation for use during pregnancy and nursing have not been established.
Pediatric use. The safety and effectiveness of neurostimulation for pediatric use have not been established.
Back pain. The safety and efficacy for the treatment of patients who have back pain as the greatest region of pain have not been evaluated.
External defibrillators. Safety for use of external defibrillator discharges on a patient receiving neurostimulation has not been established. External defibrillation can cause induced currents in the lead-extension portion of the neurostimulation system. After defibrillation, confirm the neurostimulation system is still working.
Magnetic resonance imaging (MRI). Some patients may be implanted with the components that make up a Magnetic Resonance (MR) Conditional system, which allows them to receive an MRI scan if all the requirements for the implanted components and for scanning are met. A physician can help determine if a patient is eligible to receive an MRI scan by following the requirements provided by Abbott Medical. Physicians should also discuss any risks of MRI with patients.
Patients without an MR Conditional neurostimulation system should not be subjected to MRI because the electromagnetic field generated by an MRI may damage the device electronics, cause heating at the lead tip that could result in tissue damage, and induce voltage through the lead that could jolt or shock the patient.
Computed tomography (CT). If the patient requires a CT scan, all stimulation should be turned off before the procedure. If stimulation is not turned off, the patient may experience a momentary increase in stimulation, which may be uncomfortable. Before beginning a CT scan, the operator should use CT scout views to determine if implanted or externally worn electronic medical devices are present and if so, their location relative to the programmed scan range.
For CT procedures in which the medical device is in or immediately adjacent to the programmed scan range, the operator should:
Determine the device type
If practical, try to move external devices out of the scan range
Ask patients with neurostimulators to shut off the device temporarily while the scan is performed.
Minimize X-ray exposure to the implanted or externally worn electronic medical device by using the lowest possible X-ray tube current consistent with obtaining the required image quality and by making sure that the X-ray beam does not dwell over the device for more than a few seconds.
Important note: For CT procedures that require scanning over the medical device continuously for more than a few seconds, as with CT perfusion or interventional exams, attending staff should be ready to take emergency measures to treat adverse reactions if they occur.
After CT scanning directly over the implanted or externally worn electronic medical device:
Have the patient turn the device back on if it had been turned off prior to scanning.
Have the patient check the device for proper functioning, even if the device was turned off.
Advise patients to contact their healthcare provider as soon as possible if they suspect their device is not functioning properly after a CT scan.
Diathermy therapy. Do not use short-wave diathermy, microwave diathermy, or therapeutic ultrasound diathermy (all now referred to as diathermy) on patients implanted with a neurostimulation system. Energy from diathermy can be transferred through the implanted system and cause tissue damage at the location of the implanted electrodes, resulting in severe injury or death.
Diathermy is further prohibited because it may also damage the neurostimulation system components. This damage could result in loss of therapy, requiring additional surgery for system implantation and replacement. Injury or damage can occur during diathermy treatment whether the neurostimulation system is turned on or off. Advise patients to inform their healthcare professional that they should not be exposed to diathermy treatment.
Electrosurgery. To avoid harming the patient or damaging the neurostimulation system, do not use monopolar electrosurgery devices on patients with implanted neurostimulation systems. Before using an electrosurgery device, place the device in Surgery Mode using the patient controller app or clinician programmer app. Confirm the neurostimulation system is functioning correctly after the procedure.
During implant procedures, if electrosurgery devices must be used, take the following actions:
Use bipolar electrosurgery only.
Complete any electrosurgery procedures before connecting the leads or extensions to the neurostimulator.
Keep the current paths from the electrosurgery device as far from the neurostimulation system as possible.
Set the electrosurgery device to the lowest possible energy setting.
Confirm that the neurostimulation system is functioning correctly during the implant procedure and before closing the neurostimulator pocket.
Implanted cardiac systems. Physicians need to be aware of the risk and possible interaction between a neurostimulation system and an implanted cardiac system, such as a pacemaker or defibrillator. Electrical pulses from a neurostimulation system may interact with the sensing operation of an implanted cardiac system, causing the cardiac system to respond inappropriately. To minimize or prevent the implanted cardiac system from sensing the output of the neurostimulation system:
Maximize the distance between the implanted systems;
Verify that the neurostimulation system is not interfering with the functions of the implanted cardiac system; and
Avoid programming either device in a unipolar mode (using the device’s can as an anode) or using neurostimulation system settings that interfere with the function of the implantable cardiac system
Other active implantable devices. The effect of other implanted devices, including deep brain stimulators, peripheral nerve stimulators, implanted drug delivery pumps, and cochlear implants on the neurostimulation system are unknown.
Radiofrequency or microwave ablation. Safety has not been established for radiofrequency (RF) or microwave ablation in patients who have an implanted neurostimulation system. Induced electrical currents may cause heating, especially at the lead electrode site, resulting in tissue damage.
Emergency procedures. Instruct patients to designate a representative (family member or close friend) to notify any emergency medical personnel of their implanted neurostimulation system if emergency care is required. Patients will receive an identification card to carry with them that will inform emergency medical personnel of their implanted system. Advise patients to use caution when undergoing any procedure that could include radiofrequency (RF) or microwave ablation, defibrillation, or cardioversion.
Ultrasonic scanning equipment. The use of ultrasonic scanning equipment may cause mechanical damage to an implanted neurostimulation system if used directly over the implanted system.
Therapeutic radiation. Therapeutic radiation may damage the electronic circuitry of an implanted neurostimulation system, although no testing has been done and no definite information on radiation effects is available. Sources of therapeutic radiation include therapeutic X rays, cobalt machines, and linear accelerators. If radiation therapy is required, the area over the implanted IPG should be shielded with lead. Damage to the system may not be immediately detectable.
Restricted areas. Warn patients to seek medical guidance before entering environments that could adversely affect the operation of the implanted device, including areas protected by a warning notice preventing entry by patients fitted with a pacemaker.
Component manipulation by patients. The patient must be instructed to not rub or exert pressure on implanted components through the skin as this may cause lead dislodgement leading to stimulation at the implant site, IPG inversion leading to the inability to communicate with the device, or skin erosion that can lead to another surgical procedure or possible infection.
Implantation at vertebral levels above T10. The safety and efficacy of implantation of leads implanted above the T10 vertebral level have not been evaluated.
Number of leads implanted. The safety and efficacy of the implantation of greater than four leads have not been evaluated.
Lead movement. Patients should be instructed to avoid bending, twisting, stretching, and lifting objects over 2 kg (5 lb) for at least six weeks after implantation. These activities may cause lead movement, resulting in under stimulation or overstimulation for the patient. Excessive lead migration may require reoperation to replace the leads.
Scuba diving and hyperbaric chambers. Instruct patients to avoid scuba diving and entering hyperbaric chambers above 1.5 atmospheres absolute (ATA) because these activities might damage the neurostimulation system.
Operation of machines, equipment, and vehicles. Advise patients who feel uncomfortable paresthesia during postural changes that they should not operate potentially dangerous equipment such as power tools, automobiles, or other motor vehicles. These patients should not climb ladders or participate in activities where postural changes or abrupt movements could alter the perception of stimulation intensity and cause patients to fall or lose control of equipment or vehicles or injure others.
Explosive and flammable gasses. Do not use a clinician programmer or patient controller in an environment where explosive or flammable gas fumes or vapors are present. The operation of these devices could cause them to ignite, causing severe burns, injury, or death.
Keep the device dry. Programmer and controller devices are not waterproof. Keep them dry to avoid damage. Advise patients to not use their device when engaging in activities that might cause it to get wet, such as swimming or bathing.
Device components. The use of components not approved for use by Abbott Medical with this system may result in damage to the system and increased risk to the patient.
Device modification. The equipment is not serviceable by the customer. To prevent injury or damage to the system, do not modify the equipment. If needed, return the equipment to Abbott Medical for service.
Application modification. To prevent unintended stimulation, do not modify the operating system in any way. Do not use the application if the operating system is compromised (i.e., jailbroken).
Case damage. Do not handle the IPG if the case is pierced or ruptured because severe burns could result from exposure to battery chemicals.
Cremation. The IPG should be explanted before cremation because the IPG could explode. Return the explanted IPG to Abbott Medical.
IPG disposal. Return all explanted IPGs to Abbott Medical for safe disposal. IPGs contain batteries as well as other potentially hazardous materials. Do not crush, puncture, or burn the IPG because explosion or fire may result.
Product materials. Neurostimulation systems have materials that come in contact or may come in contact with tissue. A physician should determine whether or not a patient may have an allergic reaction to these materials before the system is implanted.
Additional Warnings for Leads
Conscious sedation. The placement of the leads involves some risk, as with any surgical procedure. Conscious sedation can cause side effects such as systemic toxicity, or cardiovascular or pulmonary problems. Use caution when sedating the patient. The patient must be awake and conversant during the procedure to minimize the likelihood of nerve damage.
Preventing infection. Always remove the trial leads before implanting the implant leads to avoid the risk of infection that may cause death if the leads are not removed. Use appropriate sterile technique when implanting leads and the IPG.
Lead damage from tools. Use extreme care when using sharp instruments or electrosurgery devices around the lead to avoid damaging the lead.
Needle positioning. Always be aware of the needle tip position. Use caution when positioning the needle to avoid unintended injury to surrounding anatomical structures.
Needle insertion. When using a contralateral approach, advance the needle slowly into the epidural space and take caution as it enters. The needle will be inserted at a steeper angle than in an antegrade approach and there is a greater chance of dural puncture that will lead to a cerebrospinal fluid leak.
Advancing components. Use fluoroscopy and extreme care when inserting, advancing, or manipulating the guidewire or lead in the epidural space to minimize the risk of a dural tear. Dural puncture can occur if needle or guidewire is advanced aggressively once loss of resistance is achieved. Advance the needle and guidewire slowly. Do not use excessive force to push the lead or sheath into the neural foramen as this may result in permanent or transient nerve damage.
Removing components. Use extreme care when removing the lead stylet, the delivery sheath, and the needle to ensure that the distal tip of the lead remains in the desired location. Removing each item in slow movements while holding the remaining components in place will assist this process.
Sheath insertion warning. Insertion of a sheath without the lead may result in dural puncture. Securing the lead with the lead stabilizer will mitigate this risk.
Sheath retraction. If the sheath needs to be retracted from the epidural space, verify that the steering wing is rotated away from the needle mark no more than 90 degrees. Failure to do so may result in damage to the sheath. Before reinserting the sheath, verify there is no damage to the sheath.
Sheath rotation. If the sheath is not responding to rotation, do not rotate the steering wing out of plane from the curve of the sheath more than 90 degrees. The tip of the sheath may whip around and could cause harm to the patient.
Lead insertion through sheath. If the lead is unable to deploy out of the sheath, inject sterile water or saline slowly to release tissue that may have entered between the sheath and the lead. Do not use excessive pressure when injecting through the sheath.
Removing a kinked sheath. If the sheath has been kinked during delivery, slowly retract through the needle with the curve facing the same direction as the bevel. Failure to do so can damage or cut the lead or sheath. If resistance is encountered, pull the needle out of the epidural space and then remove the sheath.
Providing strain relief. Failure to provide strain relief may result in lead migration requiring a revision procedure.
Anchoring leads. Do not suture directly onto the lead to avoid damaging the lead. Failure to appropriately anchor the lead may cause lead migration, motor activation, or painful stimulation.
Remove leads slowly. Remove leads slowly (at a suggested rate of 1 cm/s while holding the lead between the thumb and forefinger) to avoid breaking the lead and leaving fragments in the patient. If resistance is met while removing leads from the epidural space, do not use excessive force to extract. Always perform removal with the patient conscious and able to give feedback.
Precautions
The following precautions apply to this neurostimulation system.
General Precautions
Patient selection. It is extremely important to select patients appropriately for neurostimulation. Thorough psychiatric screening should be performed. Patients should not be dependent on drugs and should be able to operate the neurostimulation system.
Infection. Follow proper infection control procedures. Infections related to system implantation might require that the device be explanted.
Implantation of multiple leads. If multiple leads or extensions are implanted, the leads and extensions should be routed in close proximity. Nonadjacent leads and extensions have the possibility of creating a conduit for stray electromagnetic energy that could cause the patient unwanted stimulation.
High stimulation outputs. Stimulation at high outputs may cause unpleasant sensations or motor disturbances, or render the patient incapable of controlling the stimulator. If unpleasant sensations occur, the device should be turned off immediately.
Postural changes. Some patients may experience a decrease or increase in the perceived level of stimulation when making postural changes. Perception of higher levels of stimulation has been described by some patients as uncomfortable, painful, or jolting. Advise patients who experience these types of stimulation changes to turn down the amplitude or turn off the IPG before making extreme posture changes or abrupt movements such as stretching, lifting their arms over their heads, or exercising. If unpleasant sensations occur, the IPG should be turned off immediately.
Advise patients about adverse effects. Instruct patients to contact their physician if they experience any adverse effects, such as unusual pain or discomfort during stimulation and swelling, redness, tenderness, or pain around implanted components.
Patient training. Instruct patients to use their neurostimulation system only after an authorized clinician has programmed the device and has trained the patient how to control stimulation and safely use the system.
Programmer use. Allow only authorized use of the clinician programmer to avoid any programming changes that may injure a patient.
Battery precaution. The clinician programmer and patient controller contain a battery and other potentially hazardous materials. Do not crush, puncture, or burn these devices because explosion or fire may result. Return them to Abbott Medical for proper disposal.
Stimulation effectiveness. The long-term effectiveness of dorsal root ganglion (DRG) stimulation has not been documented, and not all patients realize the long-term benefits from DRG stimulation. Stimulation effectiveness has been established for one year.
Sterilization and Storage
Single-use, sterile device. The implanted components of this neurostimulation system are intended for a single use only. Sterile components in this kit have been sterilized using ethylene oxide (EtO) gas before shipment and are supplied in sterile packaging to permit direct introduction into the sterile field. Do not resterilize or reimplant an explanted system for any reason.
Storage environment. Store components and their packaging where they will not come in contact with liquids of any kind.
Handling and Implementation
Expiration date. An expiration date (or “use-before” date) is printed on the packaging. Do not use the system if the use-before date has expired.
Package or component damage. Before opening any sterile package, verify the kit model number, that the kit is within its expiration (use-before) date, and that the packaging has not been damaged or compromised in any way. If the packaging has been compromised, the device is beyond its expiration date, or the sterile package or device show signs of damage, do not use the device as it may be compromised and could cause harm to the patient. Return any suspect components to Abbott Medical for evaluation.
Handle the device with care. The clinician programmer and patient controller are sensitive electronic devices that can be damaged by rough handling, such as dropping them on the ground.
Lead inspection. Carefully inspect the lead (in the sterile field) for damage after removing it from the sterile package. Damage to the lead body can cause improper function and stimulation or stimulation to areas other than the intended target.
Care and handling of components. Use extreme care when handling system components prior to implantation. Excessive heat, excessive traction, excessive bending, excessive twisting, or the use of sharp instruments may damage and cause failure of the components.
Component handling. Do not bend, kink, or stretch the lead body, sheaths, or other components as this may result in damage to the component and poor function.
Using surgical instruments. Do not use surgical instruments to handle the lead. The force of the instruments may damage the lead or stylet.
Using the tunneling tool. Use extreme care to not damage the lead with the sharp point of the tunneling tool.
Component manipulation. Do not over-manipulate the sheath and lead system as this may result in trauma within the epidural space.
Stylet handling. Do not bend, kink, or use surgical instruments on the stylet, as this may damage it. Use care when reinserting a stylet. Too much pressure on the stylet could damage the lead, resulting in intermittent or loss of stimulation. Remove the stylet from the lead only when satisfied with lead placement. If the stylet is removed from the lead, it may be difficult to reinsert it.
Sheath insertion precaution. Do not insert the sheath into the epidural space without the lead or guidewire inserted, as this may cause injury to the dura.
Stabilizing the lead during insertion. When inserting the lead-sheath assembly through the needle into the epidural space, tighten the lead stabilizer to prevent lead migration out of the sheath. Failure to do so may cause harm to the patient such as damage to the dura.
Bending the sheath. Do not bend the sheath without the lead inside the sheath, as this will permanently kink it and make it difficult to deploy the lead.
Lead handling. If the operating field is bloody, wipe gloves, lead, stylet, and sheath before handling the lead. Failure to do so may result in difficulty delivering the lead.
Exposure to body fluids or saline. Prior to connection, exposure of the metal contacts, such as those on the connection end of a lead or extension, to body fluids or saline can lead to corrosion. If such exposure occurs, clean the affected parts with sterile, deionized water or sterile water for irrigation, and dry them completely prior to lead connection and implantation.
Inserting the anchor. Failure to push the short end of the soft tissue anchor into the ligament or fascia may result in lead migration and a procedure to revise the lead location.
Securing the anchor. Use caution when securing the soft tissue anchor because damage to the anchor or lead can occur and result in failure of the system.
Placing the IPG. Do not place the IPG deeper than 4.0 cm (1.57 in) because the clinician programmer or patient controller may not communicate effectively with the IPG.
Securing the IPG. Do not bring the suture needle in contact with an IPG, lead, or extension, or the component may be damaged.
System testing. To ensure correct operation, always test the system during the implant procedure, before closing the neurostimulator pocket, and before the patient leaves the surgery suite.
Conscious sedation during removal. Always perform removal of implanted components with the patient conscious and able to give feedback.
Surgical advice for removal. If resistance is met while removing leads from the epidural space, do not use excessive force to extract. Consider seeking surgical advice if you cannot easily remove a lead.
Component disposal. Return all explanted components to Abbott Medical for safe disposal.
Hospital and Medical Environments
High-output ultrasonics and lithotripsy. The use of high-output devices, such as an electrohydraulic lithotriptor, may cause damage to the electronic circuitry of an implanted IPG. If lithotripsy must be used, do not focus the energy near the IPG.
Transcranial magnetic stimulation (TMS) and electroconvulsive therapy (ECT). Safety has not been established for TMS or ECT in patients who have an implanted neurostimulation system. Induced electrical currents may cause heating, especially at the lead electrode site, resulting in tissue damage.
Transcutaneous electrical nerve stimulation (TENS). Do not place TENS electrodes so that the TENS current passes over any part of the neurostimulation system. If patients feel that the TENS device may be interfering with the neurostimulator, patients should discontinue using the TENS device until they talk with their physician.
Home and Occupational Environments
Electromagnetic interference (EMI). Some equipment in home, work, medical, and public environments can generate EMI that is strong enough to interfere with the operation of a neurostimulation system or damage system components. Patients should avoid getting too close to these types of EMI sources, which include the following examples: commercial electrical equipment (such as arc welders and induction furnaces),communication equipment (such as microwave transmitters and high-power amateur transmitters), high-voltage power lines, radiofrequency identification (RFID) devices, some medical procedures (such as therapeutic radiation, static magnetic field [SMF] therapy, and electromagnetic lithotripsy), and some medical devices (such as bone growth stimulators, transcutaneous electrical nerve stimulation [TENS] devices, dental drills, and ultrasonic probes).
Wireless use restrictions. In some environments, the use of wireless functions (e.g., Bluetooth® wireless technology) may be restricted. Such restrictions may apply aboard airplanes, in hospitals, near explosives, or in hazardous locations. If you are unsure of the policy that applies to the use of this device, please ask for authorization to use it before turning it on. (Bluetooth® is a registered trademark of Bluetooth SIG, Inc.)
Security, antitheft, and radiofrequency identification (RFID) devices. Some antitheft devices, such as those used at entrances or exits of department stores, libraries, and other public places, and airport security screening devices may affect stimulation.
Additionally, RFID devices, which are often used to read identification badges, as well as some tag deactivation devices, such as those used at payment counters at stores and loan desks at libraries, may also affect stimulation.
Patients who are implanted with nonadjacent multiple leads and patients who are sensitive to low stimulation thresholds may experience a momentary increase in their perceived stimulation, which some patients have described as uncomfortable or jolting. Patients should cautiously approach such devices and should request help to bypass them. If they must go through a gate or doorway containing this type of device, patients should turn off their IPG and proceed with caution, being sure to move through the device quickly.
Overcommunicating with the IPG. Advise patients to use their patient controller to communicate with their IPG only when needed because excessive communication with the IPG can shorten the remaining battery life.
Consumer goods and electronic devices. Magnetic interference with consumer goods or electronic devices that contain magnets, such as mobile phones and smart watches, may unintentionally cause the neurostimulation system to turn on or turn off or affect communication between the device and generator; however, it will not change the prescribed programmed parameters. Patients should be advised to keep their mobile phones and smart watches at least 15 cm (6 in.) away from the generator and avoid placing any smart device in a pocket near the generator. If a patient is concerned about a smart device interacting with their neurostimulation system, consider disabling magnet mode. For more information about setting the magnet mode, refer to the clinician programmer manual or contact Technical Support.
Adverse Effects
In addition to those risks commonly associated with surgery, the following risks are associated with using this neurostimulation system:
Unpleasant sensations or motor disturbances, including involuntary movement, caused by stimulation at high outputs (if either occurs, turn off your IPG immediately.)
Undesirable changes in stimulation, which may be related to cellular changes in tissue around the electrodes, changes in electrode position, loose electrical connections, or lead failure or breakage
Stimulation in unwanted places (such as stimulation of the chest wall)
Lead migration, causing changes in stimulation or reduced pain relief
Epidural hemorrhage, hematoma, infection, spinal cord compression, or paralysis from placement of a lead in the epidural space Cerebrospinal fluid (CSF) leakage
Tissue damage or nerve damage
Paralysis, weakness, clumsiness, numbness, sensory loss, or pain below the level of the implant
Pain or bleeding where the needle was inserted
Persistent pain at the electrode or IPG site
Escalating pain
Seroma (mass or swelling) at the implant site
Headache
Allergic or rejection response to device or implant materials
Implant migration or skin erosion around the implant
Battery failure, leakage, or both
Hardware malfunction that requires replacing the neurostimulator
Pain from a noninjurious stimulus to the skin or an exaggerated sense of pain
Formation of reactive tissue in the epidural space around the lead, which can cause delayed spinal cord compression and paralysis and requires surgical intervention (Time to onset can range 23 from weeks to many years after implant.)
Additional risks to the patients, as a result of the placement and stimulation of the lead in the area of the dorsal root ganglion (DRG), include pain from setting the stimulation parameters too high. This may occur once the lead is in place and is connected to the neurostimulator and activated. The neurostimulator is controlled by a trained operator and the starting point for the stimulation will be set to the lowest available settings. Additionally, all patients will be awake and conversant during the procedure to minimize the impact.
26-01559 MAT-2602034 v1.0 | Item approved for U.S. use only.






Chronic Pain